Understanding Osteitis Pubis
Osteitis pubis is a relatively common but often under-recognized source of groin and pelvic pain, particularly in younger athletes. As physiotherapists, we play a critical role in the assessment, diagnosis, and management of this condition. This blog will break down the causes, anatomy, populations at risk, assessment strategies, and physiotherapy treatments for osteitis pubis.
What is Osteitis Pubis?
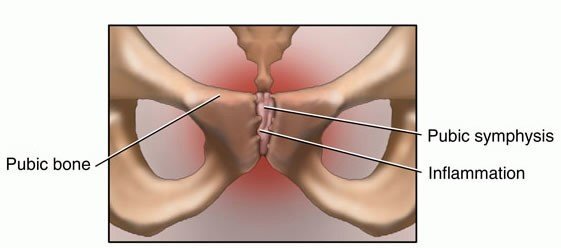
Osteitis pubis is an inflammatory condition of the pubic symphysis — The pubic symphysis is the joint at the front of the pelvis where the two pubic bones meet. This joint is supported by a complex network of ligaments and surrounded by several important muscle attachments including:
- Adductors (particularly adductor longus)
- Rectus abdominis
- Obliques
- Gracilis

Repeated stress or trauma to this region can lead to bone stress, muscular strain, and eventual breakdown of the joint, resulting in inflammation and pain in the groin area.
Mechanism of Injury
Osteitis pubis typically results from repetitive forces across the pubic symphysis. These forces are often due to:
- Rapid changes in training load or intensity which is more than what the individual can tolerate
- Repetitive twisting, cutting, or pivoting (common in football, hockey, and rugby)
- Muscular imbalances or dysfunction, particularly between the abdominal, abductor, and adductor muscle groups
- Poor core or pelvic stability
- Previous pelvic or abdominal surgery (e.g. hernia repair)
In non-athletic populations, it may also develop due to:
- Pregnancy and childbirth (due to pelvic instability)
- Urologic or gynecologic surgeries
- Biomechanical compensations
Who Gets Osteitis Pubis?
While osteitis pubis can affect a wide demographic, it is most commonly seen in:
- Male field sport athletes (e.g. AFL, soccer, rugby players)
- Female athletes involved in gymnastics, running, or netball
- Postpartum women
- People with a history of pelvic or abdominal surgeries
Athletes aged between 16–35 years are particularly susceptible due to high training loads and demanding physical activity.
Physiotherapy Assessment
A comprehensive assessment is essential to confirm osteitis pubis and rule out other causes of groin pain. Physiotherapists will perform a subjective and objective assessment to identify the cause of pain and provide strategies to fix the injury.
Subjective Assessment:
The right questions can help to identify if osteitis pubis is the source of the pain. Patients with osteitis pubis can often report the following
- Gradual onset groin or pubic pain which gets worse with activity
- Pain that lasts for hours or even days after activity – can feel dull or achy
- Worsens with kicking, sprinting, jumping, and change of direction
- Pain with coughing, sneezing, or sit-ups
- Training load increases in short periods of time
- Pain high up into the groin region, can press or specifically identify the exact spot
Objective Examination:
Following the subjective examination, if the physiotherapist suspects osteitis pubis, there is physical testing that can be done to help identify osteitis pubis
- Painful when doing sports specific activity such as running, kicking, jumping, or change in direction
- Pain reproduction with resisted adduction, hip flexion, or sit ups (e.g. squeeze test)
- Single-leg tasks or hopping may provoke symptoms
- Reduced strength or control in adductors, abductors, hip flexors, and abdominals of the affected side
- Tightness in the groin and lower abdominal region
- Palpation tenderness directly over the pubic symphysis
In some cases, referral for imaging (MRI or ultrasound) may be appropriate to confirm the diagnosis. Symptoms that happen from Osteitis Pubis can mimic other injuries. So imaging can also help to rule out other injuries such as hernia, labral tear, stress fracture.
Physiotherapy Treatment
Physiotherapy is the first-line treatment for osteitis pubis. Management typically includes the following components:
1. Load Management
- Temporarily reduce aggravating activities (e.g. running, kicking, cutting) – You can either reduce the intensity or frequency to help reduce the loading of the pubic symphysis.
- In some extreme cases, a period of absolute rest from sport and training can be necessary to allow the inflammation/bone stress settle down. This can range between 2-8 weeks depending on the severity of the injury. The earlier you can see a physiotherapist, the less time you’ll have to take off. The longer you play through the pain/symptoms, the longer you’ll have to rest. Your physiotherapist will be able to advise you on how long is an appropriate period of rest.
- Cross-training (e.g. cycling, swimming) may be used during early phases to help reduce load on the pubic symphysis, but to help keep up cardiovascular fitness.
- Gradual reintroduction of load is essential – your physiotherapist will help create a plan for you to increase your load for return to training and return to play.
2. Exercise Rehabilitation
While you are resting or reducing your load from your activity. It is important to help strengthen the muscle surrounding the pubic symphysis (Adductors, abductors, hip flexors, abdominals). Strengthening the surrounding muscles helps to reduce load on the pubic symphysis so that you can gradually increase your activity. Additionally, improving your strength will help prevent the injury from returning in the future. These exercises help to focus on:
- Hip adductor, abductor, gluteal strengthening
- Core and pelvic stability: strengthen transversus abdominis, obliques, multifidus
- Hip mobility to improve range of motion and strength in lengthened positions
- Progressive loading of the pubic symphysis to tolerate increased loading
- Address any muscular imbalances (e.g. dominant adductors vs. weak abdominals)
- Plyometric exercises to improve speed and power of the hip and core
- An introduction to running/sprinting
- Progressive sports specific exercises to improve function for sport.
3. Manual Therapy
- Soft tissue techniques for adductors, hip flexors, and pelvic musculature to help reduce pain and improve mobility
- Mobilisation of the hip, sacroiliac joints or lumbar spine if contributing
4. Biomechanical Correction
- Address faulty movement patterns (e.g. running mechanics, landing mechanics, lumbopelvic control) which could potentially increase loading on pubic symphysis
- Prescription of orthotics or footwear changes if indicated
5. Education and Return-to-Play Planning
- Clear guidance on symptom monitoring
- Gradual progression through sport-specific drills
- Communication with coaches/trainers to align return-to-play goals
Prognosis
With a structured and progressive physiotherapy plan, most patients recover fully from osteitis pubis. However, return to sport may take 6–12 weeks for most athletes. However more severe cases can take upwards of 3-9 months depending on severity and adherence to rehabilitation.
Persistent cases may require a multidisciplinary approach, including sports doctors, imaging guidance, or in rare cases, surgical consultation.
Summary
Osteitis pubis is a challenging yet treatable condition that requires a thorough and progressive rehabilitation approach. Physiotherapists are well positioned to not only help patients recover but also reduce the risk of recurrence by correcting underlying biomechanical and training issues. If you suspect you may be suffering from this condition, please reach out to us and we will do our best to ensure you get back to your activity pain free.
If you or your athletes are experiencing groin pain that won’t settle, don’t ignore it — early intervention can make a big difference.
Need help with groin or pelvic pain?
Book an appointment with one of our experienced physiotherapists to get a tailored recovery plan today.
Written by: Carlo Villadiego

