Patellofemoral Pain: How to Understand and Manage Symptoms
Patellofemoral pain (PFP) is one of the most common causes of anterior knee pain in physically active populations. It’s a multifactorial condition that demands a nuanced understanding of biomechanics, training loads, and tissue capacity.
What is Patellofemoral Pain?
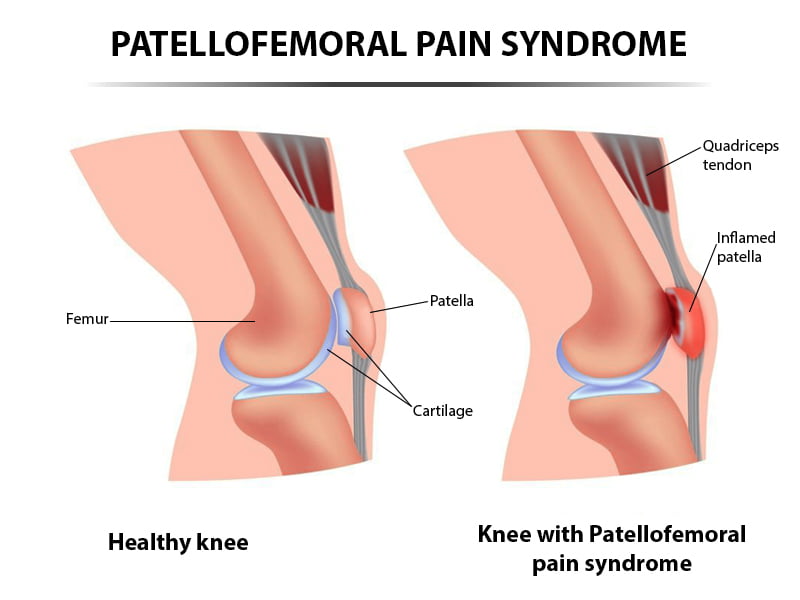
It is a type of discomfort felt at the front of the knee, around or behind the patella.
Your patella sits in a groove at the end of your femur called the trochlear groove. As you bend and straighten your knee, the patella glides up and down inside this groove.
When everything’s working well, the patella tracks smoothly. But if something disrupts this balance — like muscle weakness, poor movement patterns, or trauma — the underside of the patella or the groove itself can become irritated, as it may not be tracking as smooth as before.
Mechanism of Injury
PFP typically develops through non-traumatic, repetitive overload of the patellofemoral joint. Key contributors include:
- Excessive joint compression during knee flexion angles of 60–90°, especially in squatting, stair descent, and running.
- Malalignment and altered patellar tracking, such as lateral tilt or superior shift, often linked to quadriceps imbalance and tight lateral structures.
- Muscle imbalances, particularly weakness in the gluteus medius and quadriceps.
- Training errors, including rapid increases in volume or intensity, poor recovery, and inappropriate footwear.
These factors increase subchondral bone stress and stimulate nociceptors, contributing to persistent anterior knee pain. It is important to note that it can develop after trauamtic events, especially in older populations.
Incidence and Prevalence
PFP is highly prevalent across athletic and general populations:
| Population | Prevalence / Incidence |
| General adult population | 22.7% annual prevalence |
| Adolescents | 28.9% annual prevalence |
| Female adolescent athletes | 22.7% point prevalence |
Physiotherapy Assessment
Subjective Assessment
Patients with PFP can often present with or report the following:
- Pain Location: typically diffuse knee pain, changing locations and not always isolated within the anterior knee
- Onset: gradual, often linked to increased activity.
- Aggravating Factors: walking up and/or down stairs, squatting, running, prolonged sitting, and kneeling are some activities which can increase presence of symptoms
- Training History: recent changes in volume, intensity, or surface
- Footwear : symptoms can present after recent changes or deterioration of current footwear
- Many clients will experience patella maltracking, with the following being biomechanical causes:
- Overactive lateral quads
- Weak VMO
- Dynamic Knee Valgus
- Patients can also report of leg giving way:
- Pain causes the quadricep to not activate, leading to the joint giving way
- Pain causes the quadricep to not activate, leading to the joint giving way
These insights help differentiate PFP from other knee pathologies and guide load management strategies.
Objective Assessment
Key clinical tests and observations include:
- Pain reproduction during squatting
- Tenderness or pain on palpation of antero-medial patella
- Pain during resisted knee extension
- Reduced dynamic knee valgus and/or hip control, possibly replicating pain related symptoms
- Reduced abductor, external rotator, or quadriceps strength on affected side.
- Reduced muscle bulk on affected side
- ITB, hamstrings, and quadriceps length which is limite
- Pain when walking on stairs
- Going up will hurt less than going down.
- Going up will hurt less than going down.
NOTE: Adding medial glide during movements should resolve symptoms during movement
High-quality guidelines recommend combining hip and knee-targeted assessments to identify proximal contributors to patellofemoral joint stress.
Physiotherapy Treatment
Exercise Rehabilitation
Exercise is the gold standard intervention for PFP, with strong evidence for improving pain and function. Below are some exercises which can be incorporated to address impairments and pain:
- Hip-focused exercises: Strengthening gluteus medius/maximus and external rotators
Examples: Side-lying hip abduction, clamshells, single-leg bridges, Captain Morgan Holds, side plank - Quad-focused exercises: Targeting quadriceps, especially VMO
Examples: Terminal knee extensions, wall sits, step-downs, seated leg extensions, Spanish squats, lunge holds, front-foot or rear-foot elevated split squats. - Progressive loading: From isometric to isotonic to eccentric-focused tasks based on symptom response.
Combined hip and knee strengthening yields superior outcomes compared to isolated knee exercises.
Source: BJSM Best Practice Guide (2018)
Load Management
Managing the loads going through the knee can be a crucial factor in affecting ability to continue engaging in activities or cease due to severity of symptoms. Below are some methods to address issues related to loads:
- Activity modification: Reduce aggravating tasks while maintaining general conditioning
- Relative rest: Shift to low-load activities like cycling or pool running
- Monitoring training volume: Use RPE scales and weekly load tracking, to understand what intensity lead to aggravation of symptoms
- Return-to-play protocols: Gradual reintroduction of sport-specific drills, progressing intensity of drills or sessions accordingly.
Manual Therapy
Whilst research is mixed on its solo effectiveness, manual therapy may offer short-term relief when combined with exercise. Below are some methods that can be incorporated:
- Patellar Mobilizations: Medial glides or tilts during movements
- Soft Tissue Techniques: Myofascial release for ITB, quadriceps, lateral retinaculum, aiming to address any muscle length deficits
- Joint Mobilizations: Lumbar or hip mobilizations if regional interdependence suspected
- Patella Taping – Alters patellar alignment and reduces pain during activity
- Foot Orthoses – Useful for excessive pronation or poor foot mechanics
- Bloof Flow Restriction (BFR) – This aims to increase blood flow during low load activities, and can be a beneficial tool for those with muscle bulk issues.
Summary
Patellofemoral pain is a common and treatable condition. Whether you’re an athlete, a growing adolescent, or someone dealing with knee pain from daily activity, understanding the underlying mechanics is key to recovery.
With the right physiotherapy approach—combining targeted exercise, load management, and supportive techniques like taping or manual therapy—most people can reduce pain, improve strength, and return to the activities they love. If you’re experiencing knee pain, don’t wait for it to worsen.
Book an appointment with one of our physiotherapists to get a tailored recovery plan today!
Written by Navraj Bhogal

